Pregnancy Complications
Infant- and Family-Centered Developmental Care
Respiratory Infections
Neonatal Eye Health
Hygiene
Rare Diseases
The “Do’s and Don’ts in Neonatology” congress is a groundbreaking event dedicated to advancing neonatal care. Co-organized by GFCNI and the Union of European Neonatal and Perinatal Societies (UENPS), this congress brings together physicians, nurses, midwives, and patient and parent representatives to share knowledge, exchange ideas, and collaborate on best practices.
The program covers essential topics including immediate skin-to-skin contact, mother-newborn couplet care, parenteral nutrition, and RSV prevention. Workshops and presentations focus on practical, evidence-based approaches to ensure the best possible outcomes for preterm and sick newborns.
Held in non-jENS years, this event highlights GFCNI’s commitment to fostering innovation, collaboration, and family-centered care in neonatal health.
Join us and be part of an inspiring community shaping the future of neonatal care - one best practice at a time!
The “Do’s and Don’ts in Neonatology” congress in Ljubljana, Slovenia, marked an important milestone as a first-of-its-kind event bringing together doctors, nurses, midwives, and patient and parent representatives to explore best practices in neonatal care.
Co-organized by EFCNI (GFCNI) and the Union of European Neonatal and Perinatal Societies (UENPS), the congress addressed a wide range of essential topics, including immediate skin-to-skin contact, mother-newborn couplet care, parenteral nutrition, and RSV prevention.
Participants engaged in interactive workshops and expert-led presentations, exchanging knowledge and practical strategies to improve outcomes for preterm and critically ill newborns.
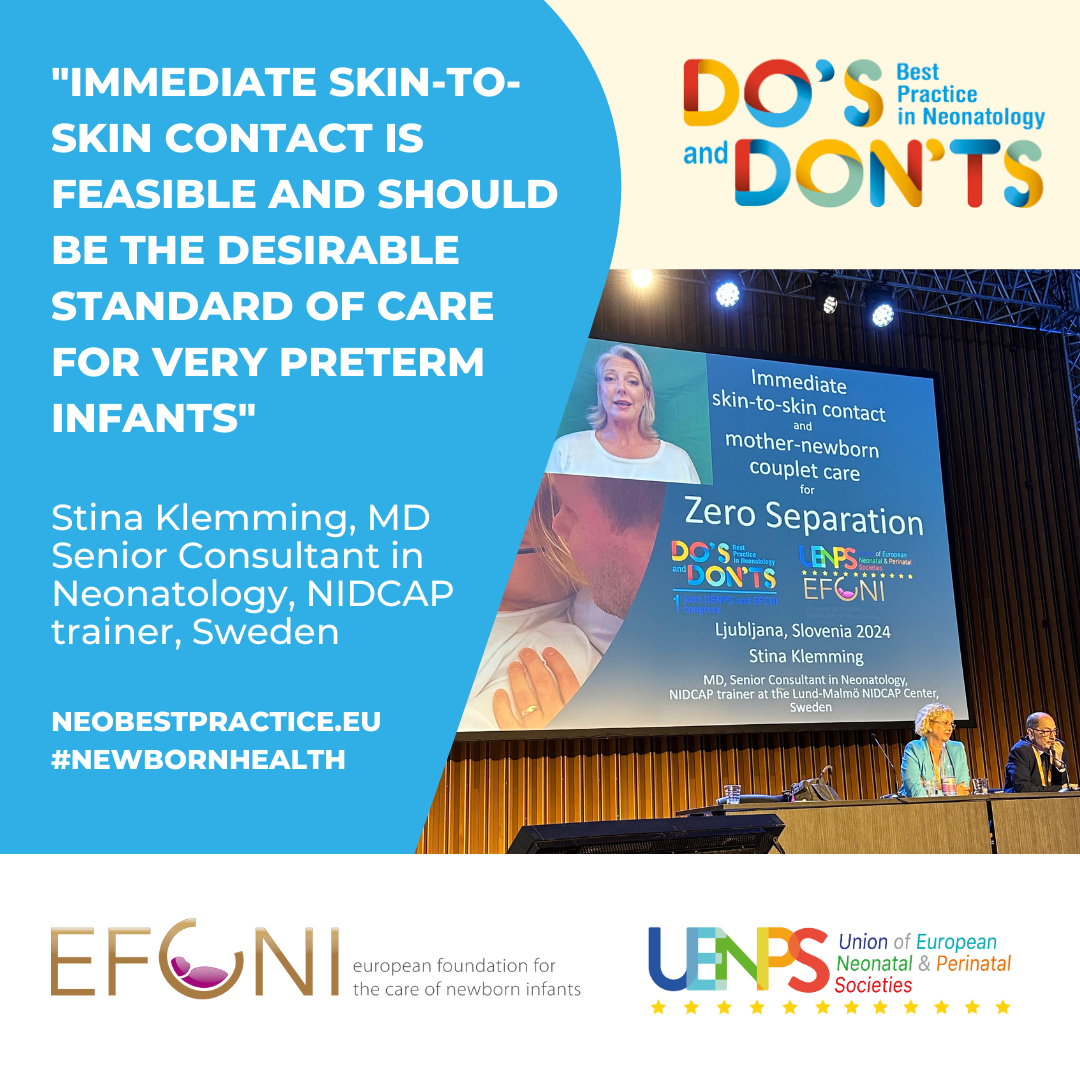
A key highlight of the first day of the “Do’s and Don’ts in Neonatology” congress in Ljubljana was a powerful and informative presentation by Dr. Stina Klemming on immediate skin-to-skin contact and mother-newborn couplet care.
Dr. Klemming shared the latest evidence and recommendations from the Immediate Parent-Infant Skin-to-Skin Study, emphasizing the proven benefits for very preterm infants and outlining essential safety practices. She stressed the importance of keeping mothers and babies together through couplet care, a practice that strengthens emotional bonds and leads to significantly improved health outcomes for both mother and child.
This session underscored the need to support care practices that keep newborns close to their parents from the very beginning. Such approaches are critical for delivering high-quality, family-centered neonatal care and promoting the well-being of newborns.
To learn more about this essential aspect of neonatal care, explore our related resources on Kangaroo Mother Care (KMC).
On the second day of the “Do’s and Don’ts in Neonatology” congress, the program focused on the critical importance of nutritional fortification for preterm and medically fragile infants.
A series of expert presentations emphasized the need for these vulnerable babies to receive additional proteins, fats, carbohydrates, and calories - nutritional elements that breast milk alone may not provide in sufficient quantities. Fortifying breast milk has been shown to be an effective and evidence-based method for meeting the unique nutritional needs of preterm and ill infants.
Silke Mader, Chairwoman of EFCNI (GFCNI), introduced a comprehensive factsheet developed specifically for parents and caregivers. This resource offers clear, accessible information on the application, types, and components of nutritional fortification, with the goal of supporting optimal growth and development in preterm and sick newborns.
The day reinforced the importance of educating and empowering families, alongside healthcare professionals and patient and parent representatives, to ensure every baby receives the best possible start in life.
The final day of the “Do’s and Don’ts in Neonatology” congress placed a strong spotlight on the critical role of parenteral nutrition (PN) for very preterm and sick newborns.
Parenteral nutrition is a life-saving method of delivering essential nutrients—such as proteins, fats, carbohydrates, vitamins, and minerals—directly into the bloodstream through a small needle or catheter, bypassing the digestive system. This approach is especially important during the first 1,000 days of life, a crucial period for ensuring optimal metabolic, cognitive, and neurodevelopmental outcomes.
For preterm infants who need more time for their digestive systems to mature, PN provides the necessary nutritional support to sustain growth and development. It is also essential for infants affected by digestive tract conditions such as necrotizing enterocolitis (NEC), which impair nutrient absorption.
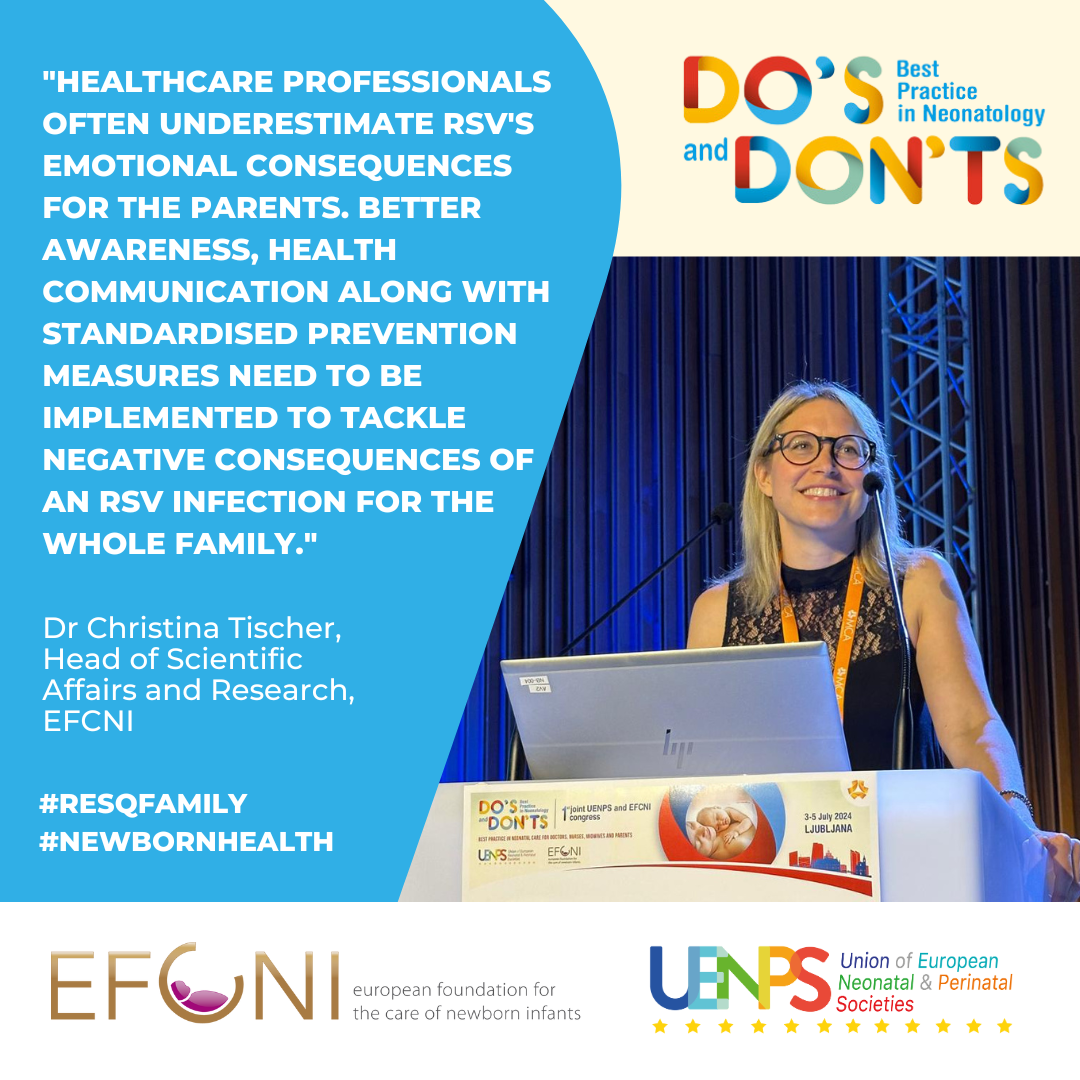
The congress concluded with a plenary session on RSV and prevention strategies. Dr. Christina Tischer and Ilona Trautmannsberger, project managers of EFCNI’s (GFCNI) ResQ Family project, presented findings on the impact of RSV infections and hospitalizations on families. Their research revealed that more than 44% of parents reported feelings of guilt for not being able to prevent their child’s RSV infection - highlighting the urgent need for better prevention strategies, increased awareness, and stronger support systems for affected families.
The day - and the congress - reinforced the value of collaboration among healthcare professionals, patient and parent representatives, and researchers to improve care and outcomes for newborns and their families.
© 2026 GFCNI. All Rights Reserved.