Pregnancy Complications
Infant- and Family-Centered Developmental Care
Respiratory Infections
Neonatal Eye Health
Hygiene
Rare Diseases
BronQ Family is an international research project studying how Bronchopulmonary Dysplasia (BPD), also known as chronic lung disease of prematurity, affects children and their families' quality of life over time.
To do so, we are inviting parents or caregivers of children born preterm (before 37 weeks of pregnancy) of both groups
to take part in an online questionnaire on families' quality of life.
We want to learn more about the challenges families face when a child is born preterm, and which experiences are specifically linked to BPD. Even if your child wasn’t diagnosed with BPD but had breathing difficulties, needed oxygen, or required ventilation after birth, your experience is highly valuable for this research.
Share Your Experience and Help Future Families
Who Can Take Part?
We invite you to participate in this survey if you are a parent or primary caregiver of a child who…
Get Involved
Share your story. Medical research depends on you to make a real difference.
Take part in the BronQ Family study by completing our online questionnaire, available in your local language. This survey takes around 30 minutes. You can pause and continue anytime.
Data Protection and Contact
Your data will be stored anonymously and according to the General Data Protection Regulation (GDPR) in Europe.
Questions? Contact us at: research(at)gfcni.org
Bronchopulmonary Dysplasia (BPD), also known as (neonatal) chronic lung disease of prematurity, is one of the most common chronic lung conditions in preterm infants, especially those born before 32 weeks of gestation or weighing less than 3.3 pounds (1,500 grams).
Although medical advances have improved survival for very preterm babies, their lungs are often not fully developed at birth. Many need help breathing, such as oxygen or a ventilator, during their first months of life. While this support is essential, it can also affect how the lungs develop, leading to BPD.
Children with BPD may continue to experience breathing problems, frequent respiratory infections, or asthma-like symptoms as they grow older. But the impact is not limited to the child. Families may face increased stress, anxiety, and financial challenges due to ongoing medical appointments, specialist care, and potential hospital readmissions.
Despite the serious nature of BPD, its long-term effects are still under-researched. Most existing studies focus on the neonatal period and early childhood, looking at issues like lung function and neurodevelopmental delays. However, we still know too little about how BPD affects families during later childhood, adolescence, and early adulthood, especially when it comes to family dynamics, parental mental health, and the economic burden of care.
Understanding the long-term impact of BPD is key to improving follow-up care, developing targeted interventions, and shaping public health policies that ease the burden on both families and healthcare systems.
The BronQ Family project is designed as an international study aiming to understand how BPD in preterm born children impacts families over time. The study will run until approximately December 2026, with data collection taking place via an online survey from September 2025 to February 2026. Ensuring a broad geographical distribution, participants living in France, Germany, Italy, Spain, the Netherlands, the United Kingdom (including Northern Ireland), and the United States are enrolled in the study. The questionnaire takes about 30 minutes to complete and will be available in English, Dutch, French, German, Italian, and Spanish.
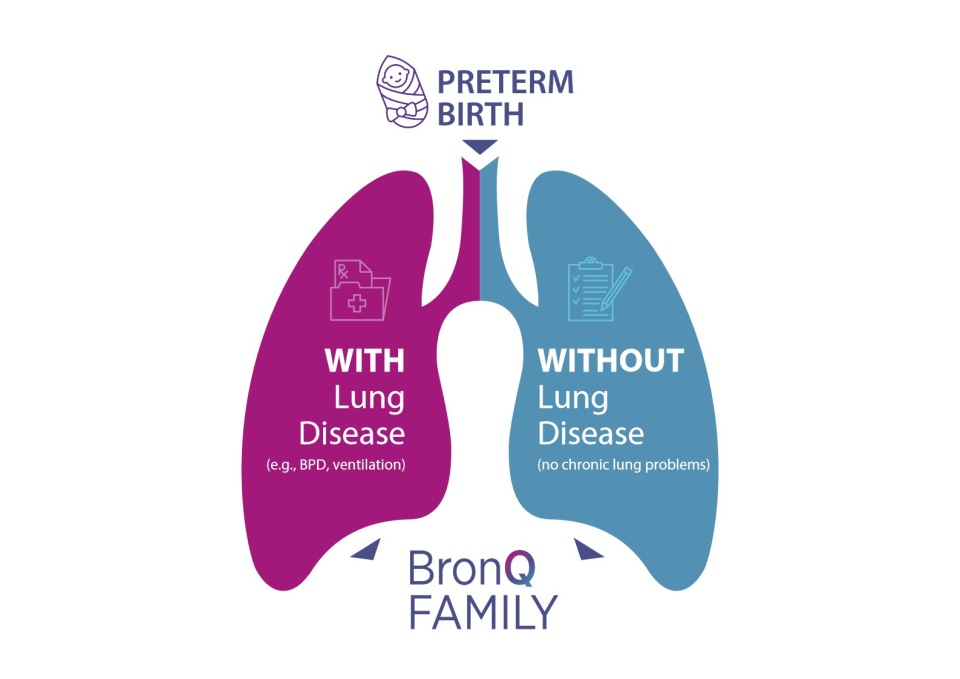
We invite parents and primary caregivers of children (from discharge of their initial hospital stay after birth from birth up to under 18 years) who were born preterm (before 37 weeks of pregnancy) – both those who have experienced BPD/respiratory or lung problems and those without a BPD diagnosis/ respiratory or lung problems – to take part in the survey.
By comparing these groups of preterm born children with and without lung problems, we aim to better understand the full picture: which challenges are specifically linked to BPD, and how they differ from the broader experiences of families with preterm children.
The project is a close collaboration with international experts and healthcare professionals, scientific advisors, healthcare societies, educational institutions, and parent organizations.
The main goal of our study is to understand how Bronchopulmonary Dysplasia (BPD) affects families over time. Key areas of focus include physical health, emotional well-being, social relationships, daily functioning, and the financial and medical challenges faced by families.
We aim to generate strong scientific evidence on the long-term effects of BPD on family quality of life as children grow into adolescence and adulthood. The results will help us to raise awareness among healthcare professionals, patient advocates, policymakers, the public, and future families.
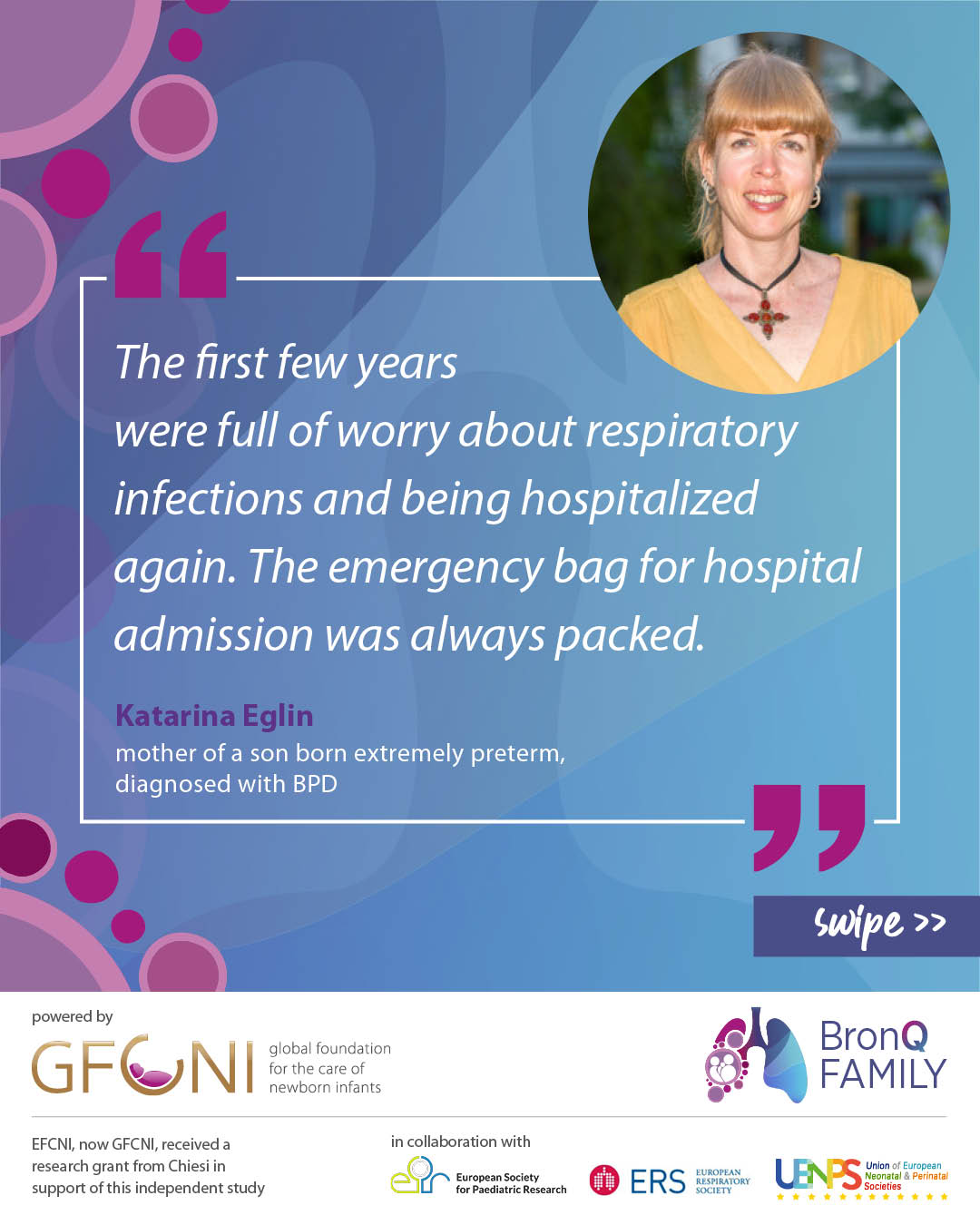
“The first few years were full of worry about respiratory infections and being hospitalized again,” says Katarina Eglin, mother of a son who was born extremely preterm and diagnosed with Bronchopulmonary Dysplasia (BPD).
“The older sister was also severely restricted at home at the beginning, because meeting friends from kindergarten in the afternoon or at the weekend could only take place outside in order to better protect the youngest from potential infection in the home environment. In the early years, children's birthday parties always had to be celebrated at the grandparents' house.”
“It took a long time for us to believe that a cold in the youngest child could simply remain a cold. The emergency bag for hospital admission was always packed.”

Sophie Proud was born as the surviving twin at just 24 weeks and had a turbulent start in life. She spent 10 weeks on a ventilator, battled repeated infections, and needed oxygen support for the first 14 months. Her parents were told to keep her away from other children to protect her fragile lungs from further infections.
As she grew, the effects of her high-frequency ventilation, high pressures, long-term oxygen at home, and severe Bronchopulmonary Dysplasia (BPD) continued to shape her childhood. She couldn’t run or play like other kids. At age 7, her lung function was still only 65–70% of normal. “I just felt like I was missing out,” Sophie remembers.
But her story didn’t end there. Today, Sophie is an adult and a NICU nurse, caring for babies like she once was. Despite everything, her most recent tests show healthy lungs, and a total lung capacity of 98%.
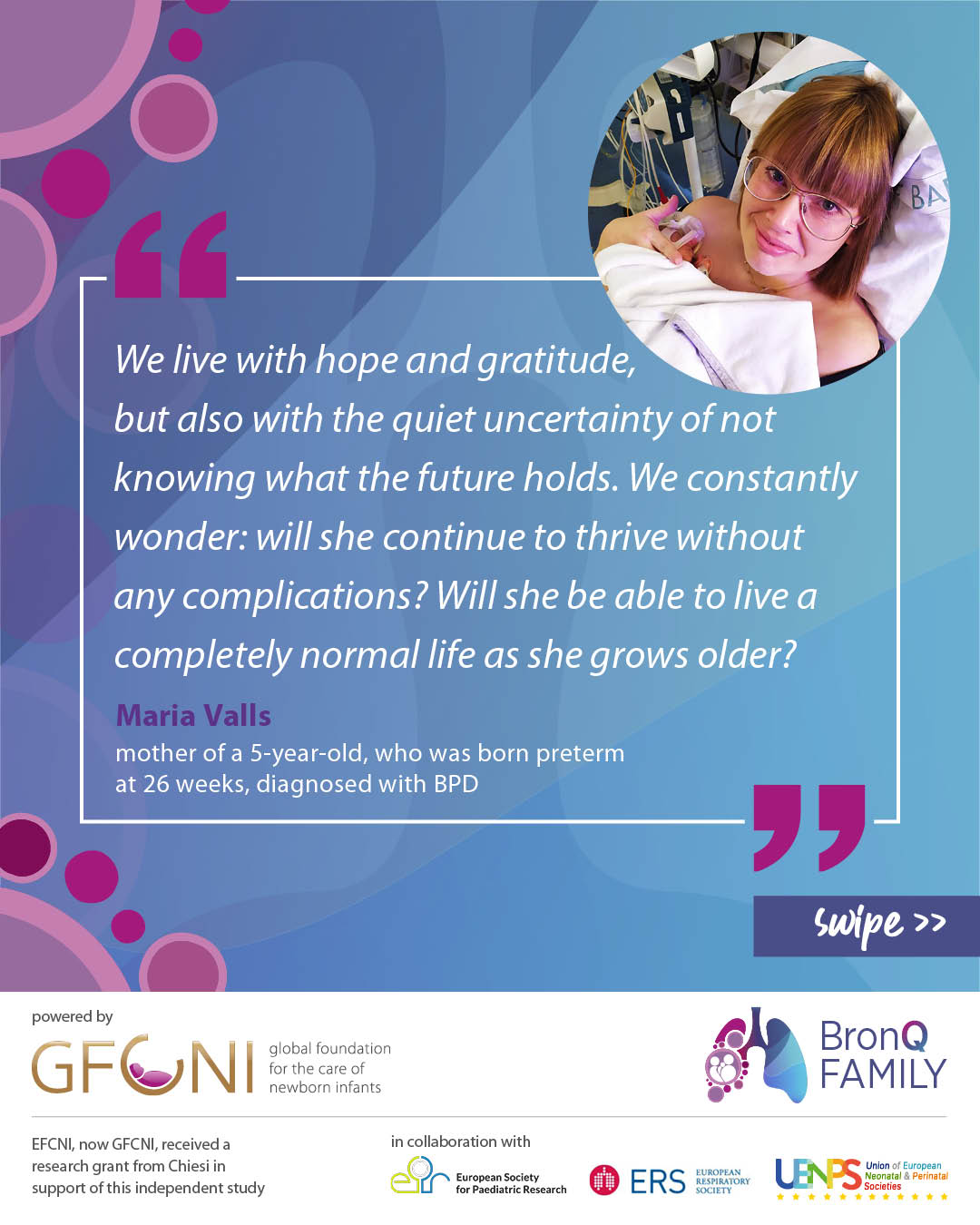
“Our daughter was born extremely premature at just 26 weeks of gestation. From the very beginning, breathing was her biggest challenge,” says Maria Valls, mother of a now 5-year-old child, who was diagnosed with Bronchopulmonary Dysplasia (BPD). “She needed to be intubated and required respiratory support for a long time in the neonatal intensive care unit. Those were very hard and uncertain days, filled with machines, alarms, and constant fear.”
“After almost four months in the hospital, we were finally able to take her home – but not without oxygen support. For the first two months at home, she still needed oxygen 24/7. It was a time of joy because we were finally together as a family, but also of stress and anxiety, as we had to manage medical equipment and monitor her constantly.”
“Now, our daughter is five years old. She is doing well and lives a seemingly normal life. We go for yearly check-ups with the pulmonology team, but we still have so many unanswered questions. No one has ever clearly told us whether she will have long-term effects from the Bronchopulmonary Dysplasia (BPD) or not. As a family, this uncertainty stays with us. We constantly wonder: will she continue to thrive without any complications? Will she be able to live a completely normal life as she grows older?”
September 2025: The Questionnaire Is Now Live!
We are excited to share that the survey is now open! This marks another important milestone in our BronQ Family project. Now we hope for many families to take part in the study and share their experiences. Every response helps us better understand family life with a chronic lung disease after prematurity, and improve care and support in the future.
We sincerely thank everyone who contributed to making this possible! Together, let's spread the word and reach as many families as possible.
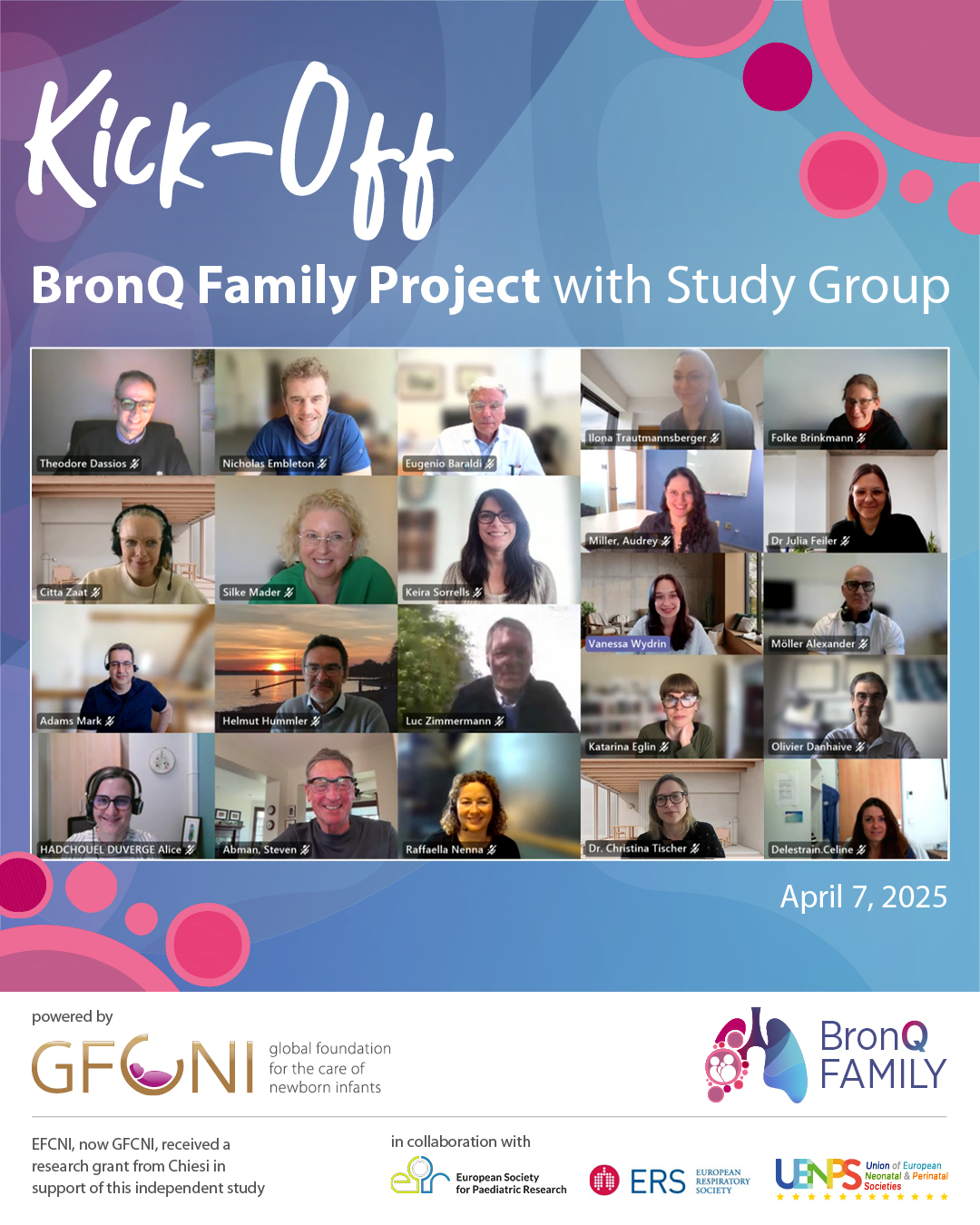
April 2025: Official Launch
A key milestone for our project: April marked the official launch of our multinational research initiative with the inaugural meeting of the Expert Study Group.
Our interdisciplinary team brings together neonatologists, pediatricians, researchers in the field of respiratory diseases and/or QoL, as well as parent and patient advocates to ensure that both scientific knowledge and lived experience shape the study’s design.
We sincerely thank everyone for their dedication and valuable contributions and look forward to the next steps. More insights and project milestones will follow – stay tuned!
BPD is a chronic lung condition that affects some babies born very early, especially those who needed help breathing after birth. These procedures are essential and lifesaving, but they can hurt the small lungs and cause long-term breathing problems.
Parents or primary caregivers of children under 18 years who were born preterm (before 37 weeks) and live in France, Germany, Italy, Spain, the Netherlands, the UK, or the US – whether the child has been diagnosed with a lung condition or not.
The person mainly responsible for the day-to-day care of the child.
Yes! All parents of preterm children under 18 can join and help us – whether or not the child has a lung condition. We value the experiences of all parents of children born preterm. By comparing results, we can better understand which challenges are specifically related to BPD.
About 30 minutes
English, Dutch, French, German, Italian, and Spanish
Your data is safe. It is stored anonymously and securely, following European data protection laws (GDPR).
Data collection runs from September 2025 to February 2026.
Your input helps us gain valuable insights on how BPD affects families’ quality of life. We aim to improve care, support, and policies for families of preterm children in the future.
We expect to finalize the results end of 2026. Check out the project’s website, follow the GFCNI social media accounts, submit to the GFCNI newsletter or contact the team.
The team of GFCNI is leading the BronQ Family project. Furthermore, an international team of researchers, doctors, and parent advocates is working together to study the long-term effects of BPD and improve support for families. Every participating country is represented by at least one parent/patient, and one medical expert. These groups help guide the project to make sure it stays relevant, respectful, and grounded in both science and lived experience. Please find further information in the sections “Project Team” and “Transparency”.
Find more information about Bronchopulmonary Dysplasia (BPD) and other possible complications of preterm or sick babies affecting the lung on the Neopedia website. Neopedia is a neonatal care encyclopedia with reliable, expert-reviewed information about preterm birth, hospitalization, and beyond.
Read more information about preventing Bronchopulmonary Dysplasia (BPD) and follow-up & continuing care in our European Standards for Care of Newborn Health.
The team of GFCNI is leading the BronQ Family project. To make sure the study reflects the real needs and experiences of families, it is conducted in close collaboration with renowned international experts, bringing together healthcare professionals, scientific advisors, and parent/patient representatives. International and local partners in the respective countries support the project.
For further information, please contact: research(at)gfcni.org
The External Scientific Advisory Board (ESAB) supports with expert guidance on study design, data interpretation, and scientific quality.
ESAB Members:
The Project Expert Group (PEG) consists of leading clinicians, researchers, and parent advocates to include both scientific rigor and real-world family needs.
PEG Members:
Healthcare Societies:
Parent Organizations:
[1] Thébaud B, Goss KN, Laughon M, Whitsett JA, Abman SH, Steinhorn RH, et al. Bronchopulmonary dysplasia. Nat Rev Dis Primer. 2019 Nov;5(1):78. https://doi.org/10.1038/s41572-019-0127-7
[2] Jensen EA, Schmidt B. Epidemiology of bronchopulmonary dysplasia. Birth Defects Res Clin Mol Teratol. 2014 Mar;100(3):145–57. https://doi.org/10.1002/bdra.23235
[3] Abman SH, Bancalari E, Jobe A. The Evolution of Bronchopulmonary Dysplasia after 50 Years. Am J Respir Crit Care Med. 2017 Feb 15;195(4):421–4. https://doi.org/10.1164/rccm.201611-2386ed
[4] Ambalavanan N, Van Meurs KP, Perritt R, Carlo WA, Ehrenkranz RA, Stevenson DK, et al. Predictors of Death or Bronchopulmonary Dysplasia in Preterm Infants with Respiratory Failure. J Perinatol Off J Calif Perinat Assoc. 2008 Jun;28(6):420–6. https://doi.org/10.1038/jp.2008.18
[5] Davidson LM, Berkelhamer SK. Bronchopulmonary Dysplasia: Chronic Lung Disease of Infancy and Long-Term Pulmonary Outcomes. J Clin Med. 2017 Jan 6;6(1):4. https://doi.org/10.3390/jcm6010004
[6] Doyle LW, Faber B, Callanan C, Freezer N, Ford GW, Davis NM. Bronchopulmonary Dysplasia in Very Low Birth Weight Subjects and Lung Function in Late Adolescence. Pediatrics. 2006 Jul 1;118(1):108–13. https://doi.org/10.1542/peds.2005-2522
[7] Harris M, Cusatis R, Malnory M, Dawson S, Konduri GG, Lagatta J. Identifying barriers and facilitators to care for infants with bronchopulmonary dysplasia after NICU discharge: a prospective study of parents and clinical stakeholders. J Perinatol. 2024 Jul;44(7):970–8. https://doi.org/10.21203/rs.3.rs-3377817/v1
[8] McGrath‐Morrow SA, Ryan T, Riekert K, Lefton‐Greif MA, Eakin M, Collaco JM. The impact of bronchopulmonary dysplasia on caregiver health related quality of life during the first 2 years of life. Pediatr Pulmonol. 2013 Jun;48(6):579–86. https://doi.org/10.1002/ppul.22687
[9] Peralta GP, Piatti R, Haile SR, Adams M, Bassler D, Moeller A, et al. Respiratory morbidity in preschool and school-age children born very preterm and its association with parents’ health-related quality of life and family functioning. Eur J Pediatr. 2023 Jan 6;182(3):1201–10 https://doi.org/10.1007/s00431-023-04829-0
[10] Feeley CA, Turner-Henson A, Christian BJ, Avis KT, Heaton K, Lozano D, et al. Sleep Quality, Stress, Caregiver Burden, and Quality Of Life in Maternal Caregivers of Young Children With Bronchopulmonary Dysplasia. J Pediatr Nurs Nurs Care Child Fam. 2014 Jan 1;29(1):29–38. https://doi.org/10.1016/j.pedn.2013.08.001
[11] Álvarez-Fuente M, Arruza L, Muro M, Zozaya C, Avila A, López-Ortego P, et al. The economic impact of prematurity and bronchopulmonary dysplasia. Eur J Pediatr. 2017 Dec;176(12):1587–93. https://doi.org/10.1007/s00431-017-3009-6
[12] van Katwyk S, Augustine S, Thébaud B, Thavorn K. Lifetime patient outcomes and healthcare utilization for Bronchopulmonary dysplasia (BPD) and extreme preterm infants: a microsimulation study. BMC Pediatr. 2020 Mar 25;20(1):136. https://doi.org/10.1186/s12887-020-02037-5
[13] Berlin KEK, Scott W, Dawson S, Brousseau D, Lagatta JM. Health-Related Quality of Life for Parents of Infants with Bronchopulmonary Dysplasia. J Pediatr [Internet]. 2024 Jan 1 [cited 2025 Mar 7];264. Available from: https://www.jpeds.com/article/S0022-3476(23)00637-6/abstract
[14] Brady JM, Zhang H, Kirpalani H, DeMauro SB. Living with Severe Bronchopulmonary Dysplasia—Parental Views of Their Child’s Quality of Life. J Pediatr. 2019 Apr;207:117–22. https://doi.org/10.1016/j.jpeds.2018.10.001
GFCNI received a research grant from Chiesi in support of this independent study. All content was independently developed and verified by GFCNI and its scientific advisors.


© 2026 GFCNI. All Rights Reserved.