Pregnancy Complications
Infant- and Family-Centered Developmental Care
Respiratory Infections
Neonatal Eye Health
Hygiene
Rare Diseases
Pre-eclampsia is a serious pregnancy complication that can affect both mother and baby. Early detection through prenatal screening is key to managing risks and improving outcomes. Learn how to recognize symptoms, understand risk factors, and take preventive steps to protect your health and your baby’s.
Pre-eclampsia—sometimes called “toxemia of pregnancy”—is a serious pregnancy complication affecting about 2 in 100 expectant mothers. Its primary symptoms include high blood pressure and elevated protein levels in the urine. Pre-eclampsia can pose significant risks to both mother and baby. While severe and early-onset cases (before 34 weeks of gestation) are rare, regular prenatal care is essential to detect the condition early and manage it effectively.
If left untreated, pre-eclampsia can progress into more severe conditions such as HELLP syndrome or eclampsia. These complications can be life-threatening for the mother, potentially leading to organ damage or even death. HELLP stands for Hemolysis, Elevated Liver enzymes, and Low Platelet count—the three hallmark symptoms of this dangerous condition.

Pre-eclampsia is one of the leading causes of preterm birth. It often restricts the baby’s growth by limiting oxygen and nutrient supply, increasing the risk of low birth weight and developmental complications. Children born to mothers with pre-eclampsia may also face an increased risk of heart and circulatory issues later in life.
For mothers, the long-term impact can be equally serious. More than 90% of women who experience severe pre-eclampsia develop chronic high blood pressure within 20 years, and many are at increased risk of cardiovascular disease. Ongoing, expert medical care and a healthy lifestyle—including balanced nutrition, regular physical activity, and stress reduction—are key to managing these risks for both mother and child.
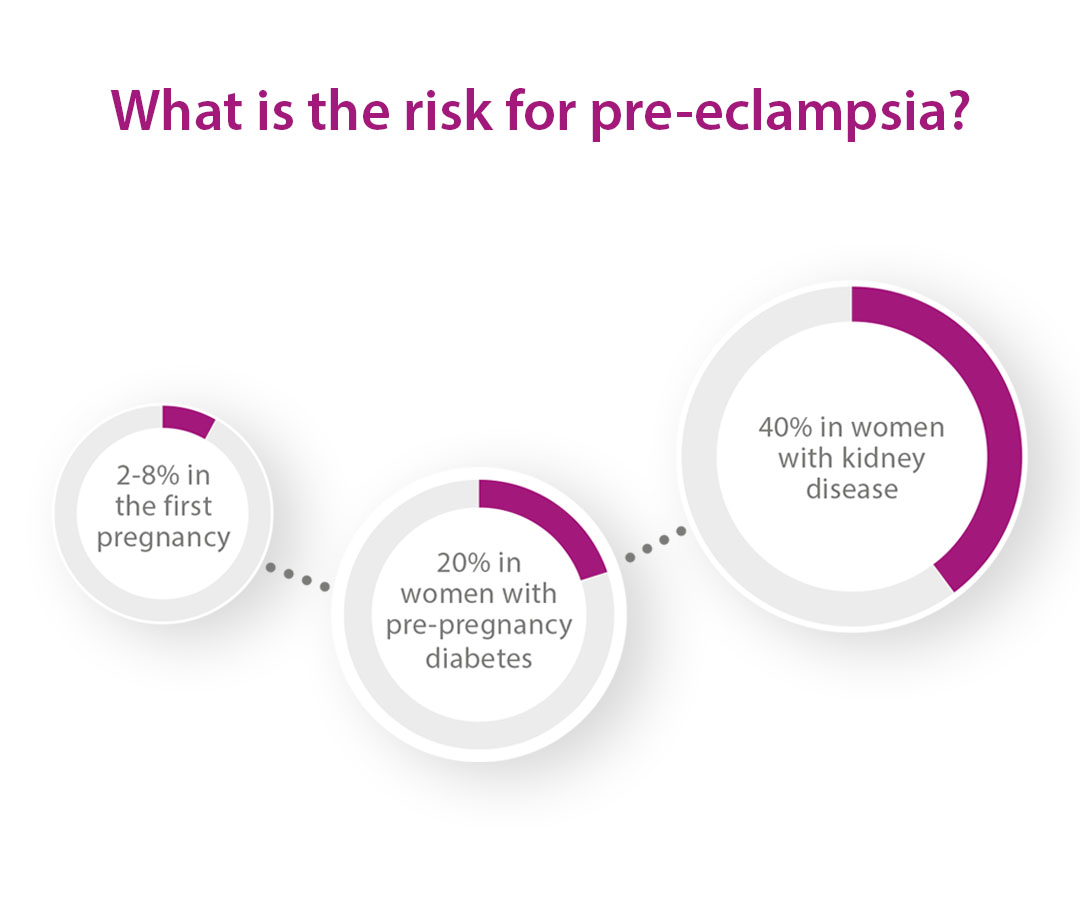
Several factors can raise the risk of developing pre-eclampsia during pregnancy. These include:
First-time pregnancy
Carrying multiples (twins, triplets, etc.)
A history of pre-eclampsia or fetal growth restriction—either in a previous pregnancy or in a close relative’s pregnancy
Pregnancy through assisted reproduction, such as artificial insemination or egg donation
Pre-existing high blood pressure
Chronic kidney disease
Diabetes or gestational diabetes
Overweight or obesity
Understanding your personal risk factors can help ensure closer monitoring and early intervention, reducing the chances of complications for both mother and baby. Regular prenatal check-ups remain the best way to identify and manage potential risks early.
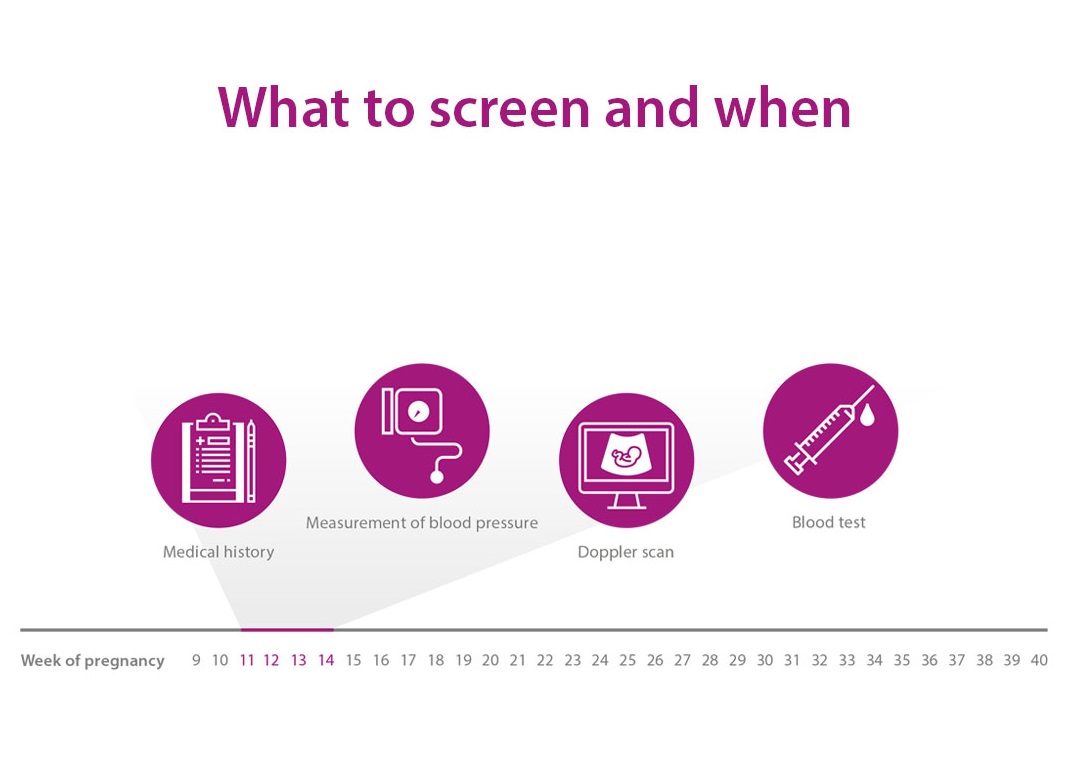
Although pre-eclampsia typically presents with high blood pressure and increased protein in the urine later in pregnancy, it actually begins developing during the first trimester—often without visible symptoms. Early screening is essential for identifying women at risk and taking preventive steps.
Between 11 and 14 weeks of pregnancy, a comprehensive screening can estimate an individual’s risk of developing pre-eclampsia. This assessment includes:
Blood pressure measurement
Doppler ultrasound to evaluate blood flow to the uterus
Maternal blood test to detect specific proteins linked to pre-eclampsia
These combined tests can identify a heightened risk well before symptoms appear. If results indicate a high risk, the healthcare provider may recommend lifestyle changes, dietary adjustments, and the use of low-dose aspirin, which has been shown to significantly reduce the risk—especially of early-onset and severe forms of pre-eclampsia.
Early detection increases the chances of receiving care from a specialized maternal-fetal medicine center, improving outcomes for both mother and baby.
In the second and third trimesters, a blood test analyzing two specific placental proteins can predict the onset of pre-eclampsia up to four weeks in advance. This allows for personalized care, including more frequent prenatal visits, if needed.
To protect their health and their baby’s, pregnant women should:
Attend all scheduled prenatal appointments
Monitor their blood pressure at home
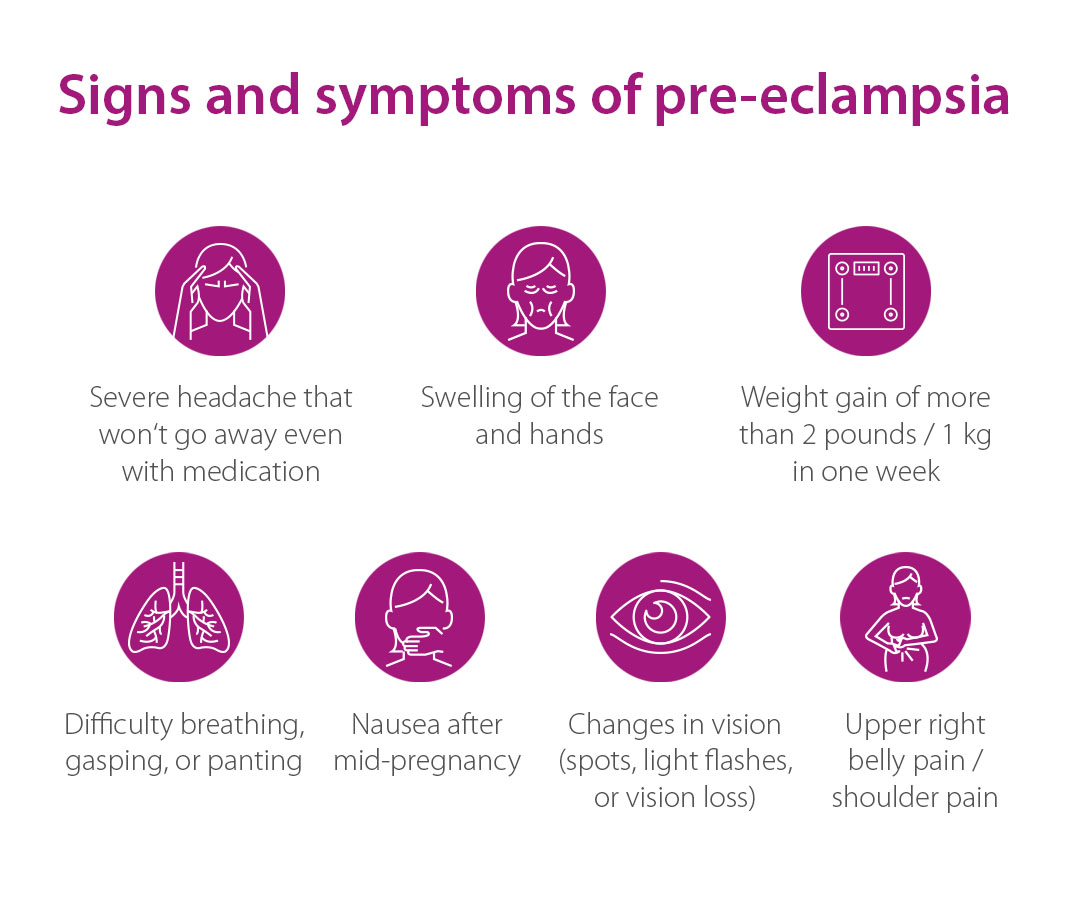
If any of these symptoms occur, it’s critical to contact a healthcare provider immediately.
Currently, the only cure for pre-eclampsia is delivery. However, in many cases, doctors aim to prolong the pregnancy safely to reduce the risks associated with preterm birth. This requires close monitoring by experienced healthcare professionals, sometimes in a hospital setting.
Expert care helps balance the health and safety of both mother and baby, ensuring timely treatment and delivery decisions.
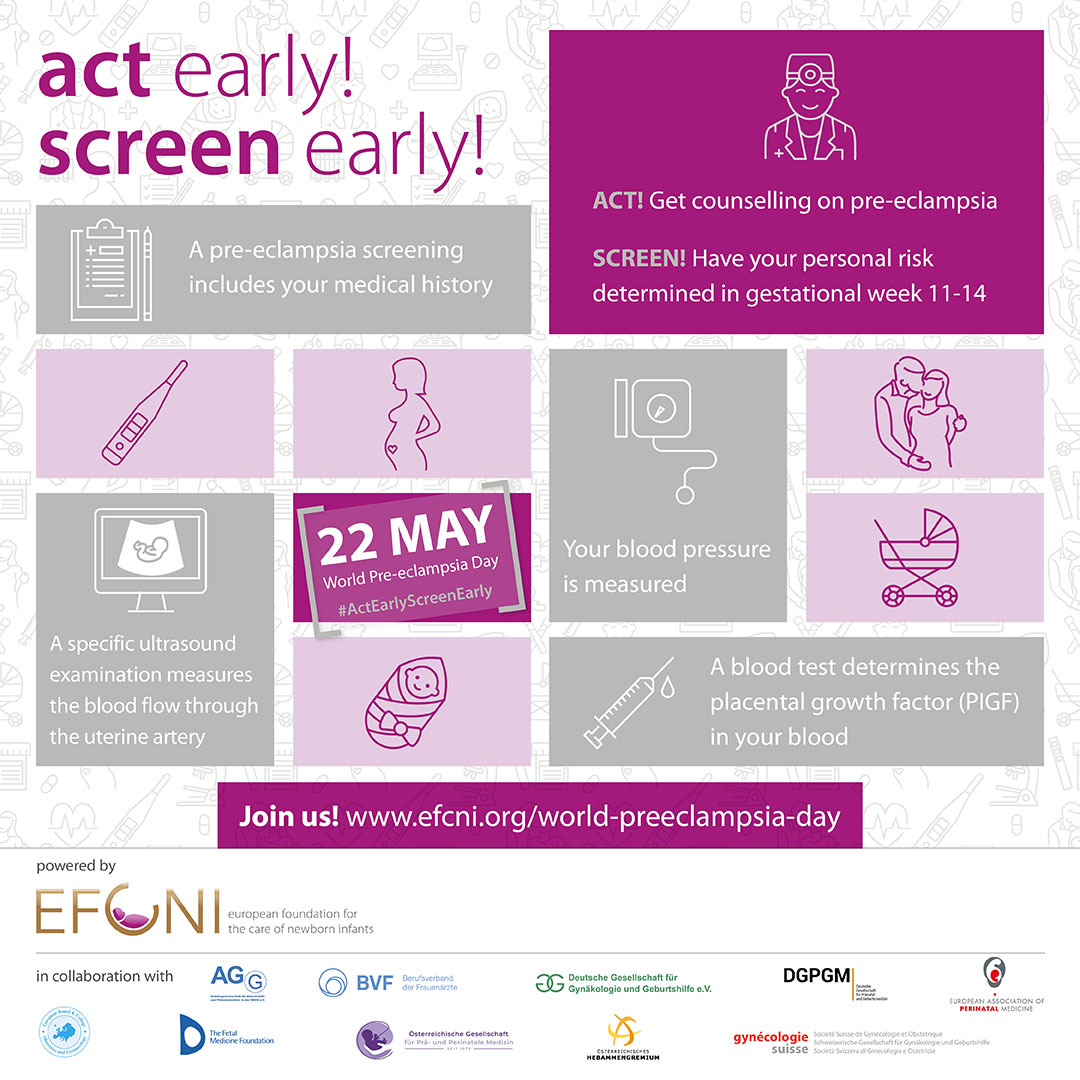
All content in the “Act Early! Screen Early!” campaign was independently developed by GFCNI and reviewed by external experts for medical accuracy. The campaign is powered by GFCNI.
We extend our sincere thanks to the following medical societies for their valuable collaboration and support of this campaign.

We thank the following parent and patient organizations for their invaluable support of this campaign around the world.

Thermo Fisher Scientific supported the campaign from 2017 to 2021 but had no influence on its content or messaging.
© 2025 GFCNI. All Rights Reserved.