
The ArtPlac project is an innovative international initiative funded by the European Innovation Council and SMEs Executive Agency (EISMEA). Launched in April 2023, the project runs for four years and brings together 10 leading research and advocacy institutions from Germany, the Netherlands, Sweden, Ireland, and Canada.
Klinikum Nürnberg leads the consortium, which includes:
Each year, approximately two million newborns die globally, many due to organ failure, particularly affecting the lungs and kidneys - a frequent complication among preterm infants [1].
Historically, medical devices and interventions used for newborns were adapted from adult care technologies, simply scaled down in size. While these approaches aimed to address life-threatening conditions, they often proved too invasive for fragile newborns, sometimes causing additional harm rather than promoting recovery [2-5].
The ArtPlac project seeks to develop a less invasive treatment method for preterm and critically ill newborns, preventing complications in vital organs.
Before birth, the placenta performs many critical bodily functions for the baby, including supporting lung and kidney function and providing nutrition. Since the placenta cannot be reconnected after birth, ArtPlac introduces a groundbreaking artificial alternative.
The ArtPlac device connects to the baby’s umbilical cord and supports both lung and kidney function - mimicking the natural role of the placenta in utero. Powered entirely by the infant’s own heartbeat, the system allows for the collection of bodily data in a far less invasive way.
This innovative device not only delivers vital health information to clinicians and supports organ function, but also creates a gentler, more natural environment that fosters healing and development.
Importantly, ArtPlac enables closer physical contact between babies and their families, overcoming the barriers posed by conventional medical equipment. This advancement supports infant- and family-centered developmental care, strengthening the emotional and physical bonds critical for early development.
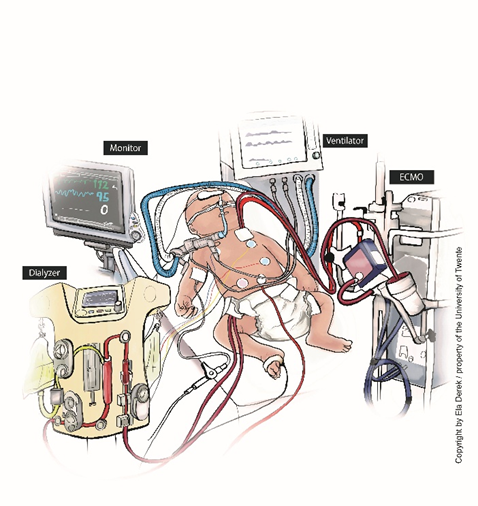
Figure 1A illustrates a typical current treatment setup for critically ill newborns, showing the extensive use of tubes, surgical lines, and monitoring equipment.
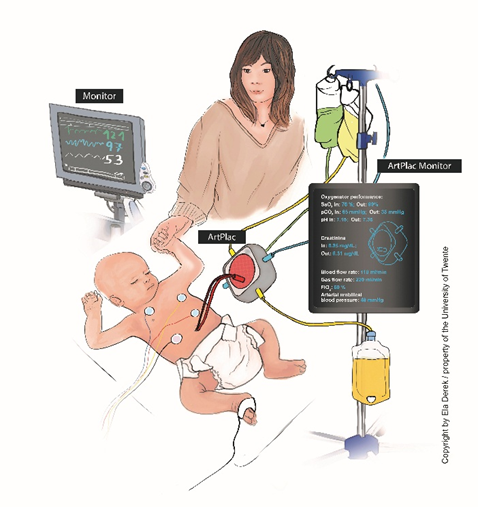
In contrast, Figure 1B presents the envisioned future using the ArtPlac device - a novel technology in development. This minimally invasive device connects to the baby’s umbilical cord and provides lung and kidney support while also monitoring vital functions in real time.
One of ArtPlac’s primary goals is to ensure parents and caregivers can stay close to their newborns throughout treatment. Involving patient and parent representatives from the start helps ensure that the device reflects the realities of hospital life and the emotional, logistical, and practical needs of families.
To that end, the Patient and Consumer Advisory Board (PCAB) - comprising five members from various geographical and professional backgrounds - joined the ArtPlac consortium for a joint Steering Committee Meeting in January 2024.
During this meeting, consortium partners presented their expertise, project status, and current challenges. The PCAB offered insightful feedback, emphasizing the importance of inclusive design and the desire to be involved in every stage of development.
Their input is helping to shape ArtPlac into a life-changing medical device that supports both clinical outcomes and family connection—a core mission shared by the entire ArtPlac team.
A key goal of the ArtPlac project is to ensure that parents and caregivers can remain close to their newborns throughout treatment. To support this, the involvement of patient and parent representatives plays a central role in every phase of the project—including the design and development of the device itself.
Hospital environments and care practices differ greatly, and so do the lived experiences of families. Gaining insight into what it means to navigate newborn intensive care - while also managing daily life and planning for the future - is vital. That’s why ongoing communication with patient and parent representatives is essential for creating a device that truly meets the needs of families.
To facilitate this exchange, GFCNI established a Patient and Consumer Advisory Board (PCAB) made up of five members from diverse geographical and professional backgrounds. In January 2024, the PCAB participated in its first joint Steering Committee Meeting with the ArtPlac consortium.
During the meeting, project teams shared their respective expertise, current progress, challenges, and findings. The PCAB members contributed valuable feedback through thoughtful questions and active discussion, highlighting key considerations for the device’s design and implementation. One particularly important message from the group: patients and caregivers want to be involved in every stage of the development process.
The ArtPlac consortium has warmly welcomed this input, recognizing that patient-centered design is essential for developing a life-changing medical device that supports both clinical excellence and family integration.
Howson, C. P. et al. Reprod Health 10, S1 (2013).
Heron, M. et al. Natl Vital Stat Rep 57, 1–134 (2009).
Stoll, B. J. et al. Pediatrics 126, 443–456 (2010).
Koyner, J. L. Et al. Blood Purif 29, 52–68 (2010).

Acknowledgment of EU Funding: This project has received funding from the European Union’s Horizon Europe research and innovation program under Grant Agreement No. 101099596.
Funded by the European Union. The views and opinions expressed are those of the author(s) and do not necessarily reflect those of the European Union or the Horizon Europe research and innovation program. Neither the European Union nor the granting authority is responsible for any use that may be made of the information contained herein.
© 2025 GFCNI. All Rights Reserved.